Molecular mechanisms underlying chronic lung disease
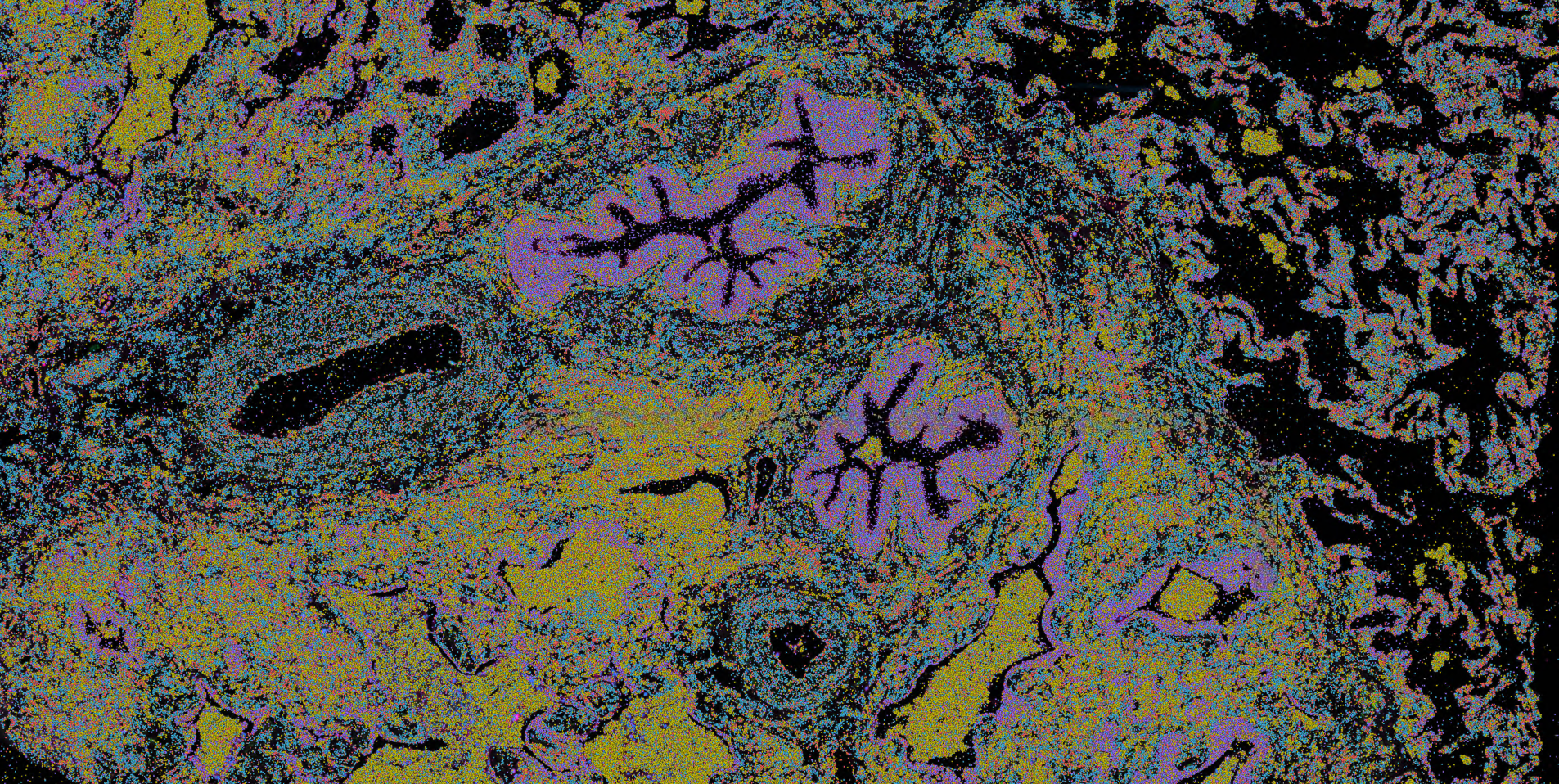
Idiopathic pulmonary fibrosis (IPF) is the most severe form of interstitial lung disease, affecting more than 50,000 Americans annually. While there are a small number of treatment options available, only a moderate impact on disease progression is obtained. Unfortunately, the majority of patients will die from respiratory failure within 3-5 years from the initial diagnosis. In collaboration with Dr. Jonathan Kropski (Vanderbilt University), we are working to map the genetics, molecular, and cellular changes associated with IPF as well as other forms of PF using both single cell and spatial transcriptomics. In collaboration with Drs. Tim Blackwell and Margaret Salisbury we are further contextualizing our findings by harnessing a one of a kind longitudinal study to characterize the changes in lungs from patients before they developed disease.
Pulmonary fibrosis affects patients later in life, however some disease features are shared with early life pulmonary conditions. Turning to neonatal disease, we are working in close collaboration with Dr. Jennifer Sucre to characterize the molecular and changes associated with bronchopulmonary dysplasia (BPD). By working on lung diseases across the lifespan we hope to better understand the molecular determinants of lung disease providing opportunities for novel biomarkers and therapeutic targets.
Finally, through these efforts we are a part of both the Human Cell Atlas and LungMap.
This work is supported by the NHLBI (U01HL175444, R01HL145372, R01HL168556, P01HL172729)
Understanding response to CAR T cell therapy at cell-type resolution in patients with brain cancer
Glioblastoma is an aggressive brain cancer affecting roughly 10,000 individuals per year in the United States. Unfortunately, fewer than 5% of patients diagnosed with GBM will survive longer than five years. Recent advances in immunotherapy - particularly CAR T therapy - have shown promise for the treatment of GBM; yet, substantial variation in response to CAR T therapy exists - in GBM as well as other tumor types. In collaboration with Dr. Christine Brown (City of Hope) we are carrying out a multi-modal and multi-omic analysis of response to CAR T cell therapy in patients with GBM. Using single cell omics we are profiling the gene expression, chromatin accessibility, and surface protein expression of the CAR T cell product, peripheral blood, cells from the cerebrospinal fluid, and tumor samples from patients undergoing CAR T cell therapy. In collaboration with Dr. Leo Wang (City of Hope) we are expanding our efforts to profile CAR T cell therapy responses in pediatric patients with brain tumors. The work in pediatric and adult brain tumors span a number of ongoing clinical trials at City of Hope with using multiple distinct CAR constructs.
This work is supported by the NCI (R01CA254271) and the V foundation for Cancer Research.
Novel approaches for single cell and spatial transcriptomics
Our lab is focused on leveraging novel genomic technologies to better understand human biology. As a part of these efforts, Dr. Banovich established TGen’s Center for Spatial Multi-Omics (COSMO). COSMO was the first center in the United States to receive the 10X Genomics Xenium as well as the the Vizgen MERSCOPE ULTA spatial transcriptomics instruments. We have devised an implemented novel tissue processing strategies to reduce cost and increase throughput. In close collaboration with Dr. Davis McCarthy, we are developing new computational approaches to identify molecular quantitative trait loci (QTL) at cell type resolution, process and analyze spatial transcriptomics data, and perform 3D analyses of spatial transcriptomics data.
This work is supported by NHGRI (R01HG011886)
Other ongoing work
We are also working on the following projects:
Functional and population genomics of Indonesia in collaboration with Dr. Herawati Sudoyo and Dr. Safarina Golfiani Malik, and Dr. Irene Gallego Romero.
Characterizing the molecular landscape of appendiceal cancers in collaboration with Dr. Mustafa Raoof.
Molecular signatures of heart transplant rejection with Dr. Ravi Shah and Dr. Kaushik Amancherla.